Ischemic Strokes and Treatment Optimization
In 2018, 1.9 million diagnosed cases of ischemic stroke in the USA, Japan, and five major EU countries were estimated. Although stroke is the second leading cause of death globally , advancements in endovascular procedures such as mechanical thrombectomy (MT) have improved clinical outcomes for stroke patients.
What is a Stroke?
Prominent in the elderly, a stroke occurs when the blood supply to a part of the brain is blocked. Strokes can be categorized as ischemic or hemorrhagic depending on their causes. Ischemic strokes, the more common of the two types (approximately 80% of all strokes), occur when there is a clot in the blood vessels supplying blood to the brain, while hemorrhagic strokes occur when weakened blood vessels rupture. It is also important to be aware of transient ischemic strokes (TIAs) or mini-strokes, as they are caused by a temporary clot that can be followed by a stroke.

Identifying Stroke?
With more than 140,000 people dying from a stroke in the United States each year, as reported by the US Centers for Disease Control and Prevention, who is the most at risk for a stroke? People who suffer from a predominant heart condition, cerebrovascular events, coronary artery disease, chronic pulmonary disease, or high blood pressure are at higher risk for a stroke; however, age, gender, family history, ethnicity and lifestyle choices are also contributing factors. Thus, being able to identify a stroke (ischemic or hemorrhagic) is critical for patient care. Stroke symptoms include weakness, paralysis of the face, arms or legs, difficulty speaking, blurred vision, and/ or a severe headache. Global healthcare providers developed the FAST method to easily identify a stroke and spread awareness amongst the public.
FAST stands for:
- F: Face drooping
- A: Arm weakness
- S: Speech difficulty
- T: Time to call (Ambulance)
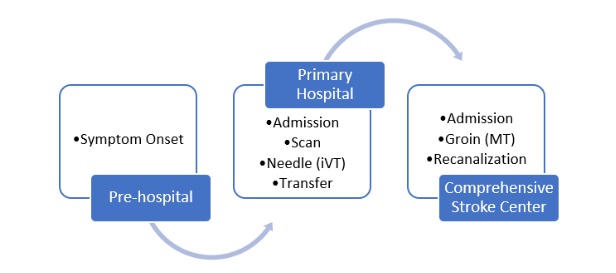
Stroke Diagnosis Pathway
Once stroke symptoms are recognized, the patient pathway begins. It starts with the patient being admitted to a primary hospital capable of scanning him/her and diagnosing the condition. This process is time sensitive as the stroke type will guide further treatment. The sooner the stroke is diagnosed, the greater the likelihood of improved clinical outcomes and patient recovery increases. Doctors will perform a series of tests to determine the patient’s risk. The first step, according to the Mayo Clinic, is that the doctor should complete a physical examination of the patient and ask a family member about the symptoms they witnessed, along with any previous signs of injury or disease. Blood tests are also essential, as they can help evaluate sugar levels, the time of blood clotting, and the balance of other critical blood chemicals. Finally, for stroke diagnosis, various imaging studies can be taken into consideration, such as computerized tomography and magnetic resonance imaging. These tests are determined by the doctor, according to the patient’s situation, and can be any of the following:
- Computerized Tomography (CT) scans are used to recognize a hemorrhage, tumor, ischemic stroke, and other conditions.
- Magnetic Resonance Imaging (MRI) can detect tissue(s) damaged by an ischemic stroke or hemorrhage.
- Carotid ultrasound can show blood flow and the build-up of fatty deposits in the carotid arteries.
- A cerebral angiogram gets a detailed view of the brain and neck arteries by injecting a dye into the blood vessels
- An echocardiogram can be used to look for clots that may have travelled from the heart to the brain, causing a stroke.
By combining the patient’s history, symptoms, blood work, and imaging studies the doctor can accurately determine the stroke type and develop a treatment plan. The possible conclusions are (1) no transient ischemic attack or stroke, (2) transient ischemic attack, or (3) acute stroke (ischemic or hemorrhagic).
Ischemic Stroke Treatment
If an ischemic stroke is diagnosed, then the direct goal of treatment is to restore blood flow to the brain. Treatment can include medications such as clot busting drugs and/ or endovascular procedures. Globally, the gold standard for treating ischemic stroke is using tissue plasminogen activator (tPA) also known as alteplase, primarily through intravenous injection. This clot busting drug is injected through the vein within 3 to 4.5 hours after stroke symptoms appear and helps dissolve the clot that caused the stroke and restore blood flow. The aim of this approach is “the quicker, the better.” Important to note is that the time window is considered the door-to-needle time, with less passing time meaning a reduced risk of complication and increased rate of survival.
On the other hand, endovascular procedures are performed directly inside the blocked vessel and have larger time windows than the intravenous approaches. One such procedure, known as intra-arterial thrombolysis, delivers tPA to the affected brain area through a long catheter that is inserted via a small incision in the groin artery. However, today’s focus is on another endovascular treatment, mechanical thrombectomy (MT), since its time window quadrupled from 6 hours to up to 24 hours. It is particularly beneficial to patients who suffer a large clot, as these clots are difficult to dissolve completely with tPA.
Mechanical Thrombectomy
Mechanical thrombectomy (MT) uses a catheter to maneuver a stent retriever through the cerebral arteries to the blocked brain blood vessel to trap and remove the clot. This interventional neuroradiological procedure is performed by trained personnel under general anesthesia or conscious sedation in an angiographic suite, commonly used for large vessel occlusion. Additionally, it can be performed in combination with intravenous tPA for effective results.
The most important aspect of mechanical thrombectomy (MT) is the time window evolution. The DAWN and Defuse 3 trials challenged the assumption of providing an interventional procedure within 6 hours of initial symptom onset, and suggest patient benefits for up to 24 hours. These studies proved a decreased degree of disability among patients who received mechanical thrombectomy (MT) treatment. This evolution, of up to 24 hours from door-to-puncture time, is a result of various trials which demonstrated massive patient benefits to those arriving late to the medical facility after symptom onset. Recent studies have suggested that this form of treatment may be the most effective for ischemic stroke, and several hospitals, including facilities like Mayo Clinic, have proven through clinical studies that decreased door-to-puncture time reflects decreased rehabilitation time and ultimately cost and resource savings for the hospital during the post-treatment phase. Furthermore, endovascular treatment research has confirmed that time is critical for patient recovery and reducing the degree of possible disability after a stroke. Now, various cases allow a door-to-puncture time as late as 24 hours after symptom onset, if the large artery occlusion is in posterior circulation.
Despite the challenges and investment to start endovascular procedures, such as an angiographic suite and a trained interventionist to perform the procedure, there has been a significant increase in the number of patients receiving these procedures.
Conclusion
Overall, there are opportunities to better treat ischemic stroke patients by improving accessibility to patients and referring them to comprehensive stroke centers that offer endovascular procedures late after symptom onset. Ischemic stroke is a major risk globally and accounts for approximately 80% of all strokes. Currently, the stroke patient pathway needs to be optimized as door-to-puncture time is key to improve outcomes and post-stroke recovery. Today, clot busting drugs are still the gold standard to treat patients, but with technological advancements and validated clinical studies, mechanical thrombectomy (MT) appears to be a promising therapy to treat strokes and considerably improve patient outcomes. All in all, mechanical thrombectomy (MT) needs to be better integrated into current patient management pathways, with the aim to provide treatment to the maximum number of qualified patients.
How can TMTG help?
To overcome the barriers of integrating a new technology, such as mechanical thrombectomy (MT), into the ischemic stroke treatment pathway requires unbiased and reliable data from the different healthcare markets and providers. The MarkeTech Group has over 20 years of experience conducting qualitative and quantitative in-depth customer insights research to help top-tier health care companies make business decision based on a comprehensive understanding of the healthcare practice and behaviors.
Contact Us
USA
The MarkeTech Group, LLC
502 Mace Blvd, Suite 15
Davis, CA 95618
Tel: (+1) 530-792-8400
Fax: (+1)
530-792-8447
France
The MarkeTech Group, SARL
3, Rue Emile Péhant
44 000 Nantes - FRANCE
Tel: +33 (0)2 72 01 00 80
Fax: +33 (0)2 40 48 29 40
Our site links
Website imagined and executed by RivalMind.




